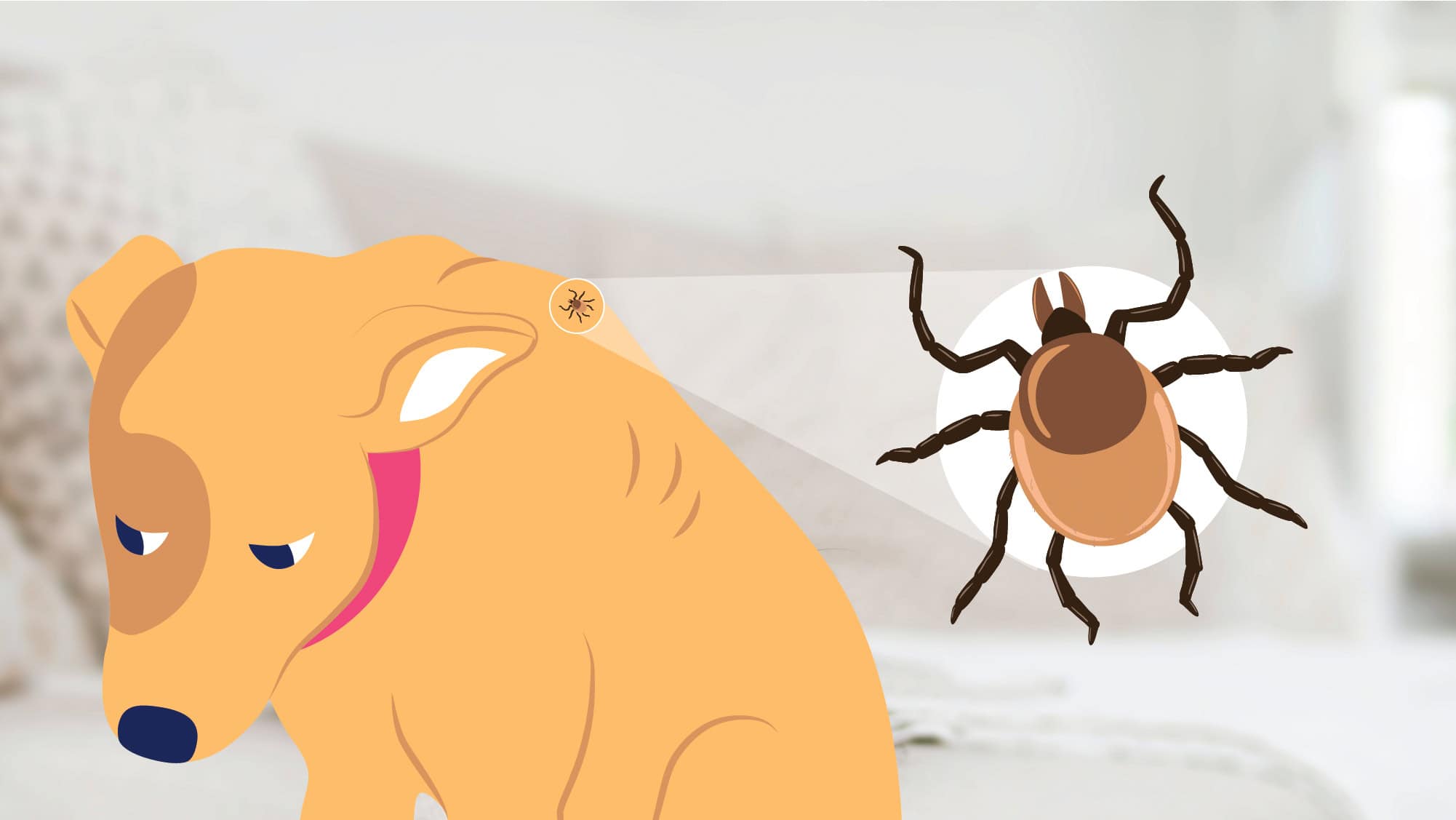
Lyme disease in dogs is caused by bacteria that can be transmitted through a bite from an infected tick.
It can cause health problems and severe illness in dogs, but it can also be tricky to diagnose. Lyme disease is more common in some regions of the U.S. than others, but as a veterinarian, I believe it is a dog health risk that I think all pet parents should know about.
What is Lyme Disease in Dogs?
Lyme disease is a bacterial infection caused by a bacteria called Borrelia Burgdorferi. It is primarily transmitted through the bite of infected ticks, specifically the black-legged tick or deer tick.
These ticks become infected by feeding on small mammals that carry the bacteria.
How is Lyme Disease Transmitted?
When an infected tick bites a dog and feeds on its blood, it can pass the bacteria into the dog’s bloodstream. Not all ticks have the bacteria, and not all tick bites lead to Lyme disease.
It usually takes around 36 to 48 hours after attaching to a dog’s body. Once the bacteria reaches a dog’s bloodstream, it can impact the joints, muscles, kidneys and heart, and cause Lyme disease symptoms.
Symptoms of Lyme Disease in Dogs
Lyme disease symptoms in dogs can have a wide range of symptoms that can be difficult to recognize. It may take weeks or months for symptoms to appear, and some dogs may not show any signs at all. Unlike humans, dogs usually don’t develop a bull’s eye rash around the tick bite.
Here are some of the most common symptoms of Lyme disease in dogs:
-
Fever
-
Swollen joints
-
Lameness (limping)
-
Swollen lymph nodes
-
Increased drinking or urination
-
Neurological symptoms
How is Lyme Disease Diagnosed?
Diagnosing Lyme disease in dogs can be challenging because the symptoms can be vague and similar to other health issues. Your veterinarian will inquire about your dog’s vaccination status and conduct a thorough examination.
Blood tests are available to aid in the diagnosis of Lyme disease. These tests detect antibodies in your dog’s blood, usually around 3-5 weeks after infection.
However, it’s important to note that these tests are not always completely reliable and may need to be repeated.
Treating Lyme Disease in Dogs
Treatment for Lyme disease in dogs primarily involves the use of antibiotics since it is a bacterial infection. The preferred antibiotic is typically Doxycycline, and your veterinarian will likely prescribe a course lasting several weeks.
It’s crucial to complete the entire course of antibiotics and schedule follow-up visits and blood tests to ensure the effectiveness of the treatment.
In some cases, dogs may also require anti-inflammatory medication and pain relief, especially if they experience joint issues. If there are any kidney problems associated with Lyme disease, appropriate treatment will be necessary.
Long-Term Effects of Lyme Disease
Long-term effects of Lyme disease in dogs can include arthritis and heart and kidney damage. Fortunately, most dogs recover well from Lyme disease.
However, it’s essential to remain vigilant for the possible recurrence of symptoms, as relapses can happen. In rare instances where Lyme disease becomes severe or leads to complications, hospitalization may be required for intensive treatment.
Preventing Lyme Disease in Dogs
To prevent Lyme disease in dogs, it is crucial to prevent ticks from attaching to your pet. It’s also essential to determine if Lyme disease is common in the area where you live and walk your dog.
Here are some simple steps you can take to protect your dog from ticks:
-
Use regular flea and tick prevention: Consult your veterinarian to find the most suitable tick prevention program for your pet. They can guide you through the different options available.
-
Inspect your dog after walks: After walking your dog, especially in woodland or areas with long grass, carefully check your pet for ticks. Ticks tend to target the head, neck, and legs.
-
Promptly remove ticks: If you find a tick on your dog, it’s important to remove it as soon as possible. Your veterinarian can demonstrate the proper technique to ensure complete removal.
-
Avoid tick-prone areas: In warmer months when ticks are more prevalent, try to avoid areas with long grass and marshes where ticks are commonly found.
Conclusion
The best way to prevent Lyme disease is using a tick preventative, like Nexgard or Bravecto, available by prescription from your veterinarian.
During an in-home Wellness Exam with BetterVet, we will discuss your dog’s vaccination schedule and whether yearly Lyme tests and vaccines are appropriate.
If your pup has had a previous diagnosis of Lyme disease, let us know so that we can continue to monitor them closely.
Frequently Asked Questions
What are the first signs of Lyme disease in dogs?
Some of the most common signs of Lyme disease in dogs include fever, swollen lymph nodes, loss of appetite, painful or swollen joints, mobility issues, and low energy.
How soon after a tick bite can a dog get Lyme disease?
Usually, a tick must be embedded on a dog for 36 to 48 hours or more before the Lyme bacteria can be transmitted.
How can you tell how long a tick has been attached?
If the tick is round and swollen, which is referred to as “engorged,” and the color has changed to gray or brown, it is likely that the tick has been attached for more than 36 hours.
Can I catch Lyme Disease from my dog?
Humans can develop Lyme disease from infected ticks, but not directly from their dogs.
Can a dog recover from Lyme disease?
Yes, most dogs recover well from Lyme disease with proper treatment and monitoring.
How serious is Lyme disease in dogs?
Lyme disease can be a serious dog illness, affecting various body systems.
Which states have the most Lyme disease?
States with the highest rates of Lyme disease include Rhode Island, Vermont, and Maine, New York, Pennsylvania, and New Jersey.
Sources:
-
Appel,M. J. G., 19920500782, English, Journal article, 0193-1903, 12, (5), Compendium on Continuing Education for the Practicing Veterinarian, (617–626), Lyme disease in dogs and cats., (1990)
-
Littman, M.P., Goldstein, R.E., Labato, M.A., Lappin, M.R. and Moore, G.E. (2006), ACVIM Small Animal Consensus Statement on Lyme Disease in Dogs: Diagnosis, Treatment, and Prevention. Journal of Veterinary Internal Medicine, 20: 422-434. https://doi.org/10.1111/j.1939-1676.2006.tb02880.x